The "Brain-Eating Amoeba": Understanding *Naegleria fowleri* and How to Stay Safe
The "Brain-Eating Amoeba": Understanding Naegleria fowleri and How to Stay Safe
Meta Description: Learn about Naegleria fowleri, the rare but deadly "brain-eating amoeba." Discover its habitats, how infections occur, symptoms of PAM, and crucial prevention tips to protect yourself.
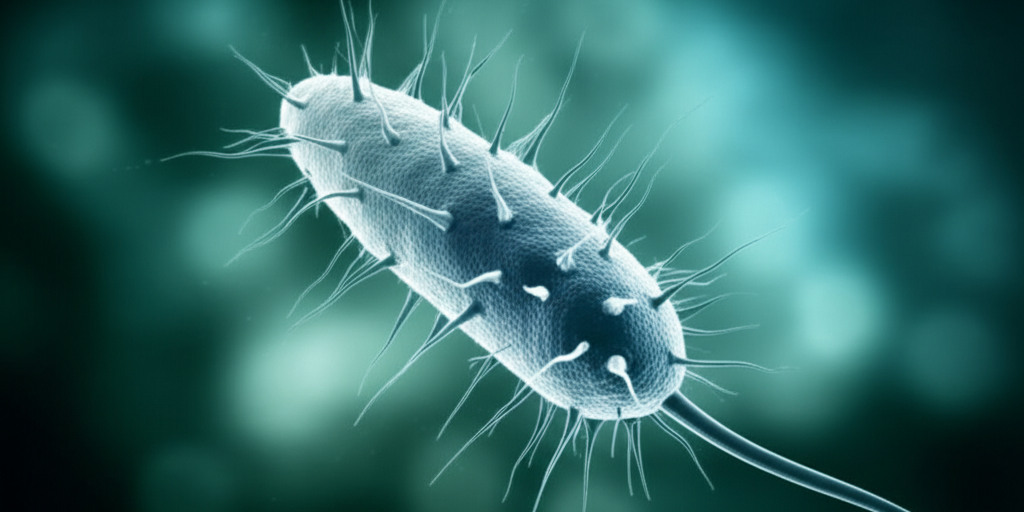
The mere mention of a "brain-eating amoeba" is enough to send shivers down anyone's spine. It conjures images of horror movies, but the reality of Naegleria fowleri is far more serious and, thankfully, incredibly rare. This microscopic organism causes a devastating infection known as Primary Amoebic Meningoencephalitis (PAM), which is almost always fatal. While fear-inducing, understanding this amoeba's nature, its preferred habitats, and—most importantly—how to prevent infection is crucial for staying safe, especially as climate patterns shift.
This comprehensive guide will demystify Naegleria fowleri, explain how it causes disease, detail its symptoms, discuss current treatment challenges, and provide actionable advice to minimize your risk.
What Exactly is the "Brain-Eating Amoeba"?
The scientific name for the "brain-eating amoeba" is Naegleria fowleri. It's a single-celled organism, a type of free-living amoeba, which means it doesn't need a human or animal host to survive. In its natural environment, Naegleria fowleri primarily feeds on bacteria. However, under specific conditions, it can become a deadly pathogen for humans, leading to Primary Amoebic Meningoencephalitis (PAM), an acute and severe infection of the brain.
Despite its alarming nickname, Naegleria fowleri doesn't "eat" your brain in the way you might imagine. Instead, once it enters the brain, it causes immense inflammation and tissue destruction, resulting in rapid swelling and ultimately, the nearly universal fatality associated with PAM.
Where Does Naegleria fowleri Live?
Naegleria fowleri is a "thermophilic" organism, meaning it thrives in warm environments. It's found worldwide in a variety of warm freshwater sources and soil.
Common habitats include:
- Warm freshwater bodies: Lakes, rivers, ponds, and hot springs are prime locations, especially during hot summer months when water temperatures rise and levels may decrease.
- Geothermal waters: Natural hot springs and warm water discharges from industrial or power plants.
- Poorly maintained or unchlorinated swimming pools: If chlorine levels are inadequate (below 0.5 mg/L), the amoeba can survive and multiply.
- Water heaters and pipes: It can colonize domestic water systems, particularly water heaters, if conditions are favorable.
- Soil: Naegleria fowleri also lives in soil, but water is the only known source of human infection.
- Tap water: In very rare instances, it has been found in municipal tap water, especially if untreated or inadequately treated well water is used, or in systems with warm water discharge.
It's important to note that Naegleria fowleri cannot survive in saltwater, like the ocean, or in properly treated, clean, and cool water.
How Do Infections Occur?
Infection with Naegleria fowleri is unique and specific: it only occurs when water containing the amoeba is forced up the nose.
This typically happens during:
- Recreational water activities: Swimming, diving, jumping, or vigorous play in warm freshwater lakes, rivers, or hot springs where water can enter the nasal passages.
- Nasal irrigation: Using contaminated (non-sterile) tap water in nasal rinsing devices like neti pots for sinus cleansing.
Once the amoeba enters the nose, it travels along the olfactory nerve fibers through the cribriform plate to the brain, where it initiates the severe infection.
Crucially, you cannot get infected by:
- Swallowing water contaminated with Naegleria fowleri.
- Person-to-person transmission.
- Water vapor or aerosol droplets (e.g., from showers or humidifiers).
Understanding Primary Amoebic Meningoencephalitis (PAM)
Primary Amoebic Meningoencephalitis (PAM) is the official name for the severe and almost always fatal brain infection caused by Naegleria fowleri. It's an aggressive disease that progresses very rapidly, destroying brain tissue and causing significant brain swelling (edema).
Symptoms to Watch For
The symptoms of PAM are often non-specific initially, resembling other more common illnesses like bacterial or viral meningitis, which can lead to diagnostic delays.
Initial symptoms typically appear between 1 to 12 days after nasal exposure, with a median onset of about 5 days. These can include:
- Severe headache
- Fever
- Nausea and vomiting
- Changes in taste and smell (less common early symptom)
As PAM progresses rapidly, later and more severe symptoms can emerge within a few days:
- Stiff neck
- Confusion
- Lack of attention to surroundings
- Loss of balance (ataxia)
- Seizures
- Hallucinations
- Coma
Death typically occurs very quickly, usually within 1 to 18 days after the onset of symptoms, with a median of about 5 days.
Diagnosis and Treatment
Diagnosing Naegleria fowleri infection quickly is one of the biggest challenges, primarily due to its rarity and the non-specific nature of early symptoms. Most diagnoses have historically been made post-mortem.
When PAM is suspected, healthcare providers look for the amoeba in:
- Cerebrospinal fluid (CSF): Obtained via a spinal tap (lumbar puncture), this fluid can be examined under a microscope for direct visualization of the amoeba.
- Brain tissue: A biopsy can be taken and examined.
- Specialized laboratory tests: These include polymerase chain reaction (PCR) tests to detect Naegleria fowleri DNA, and immunohistochemical (IHC) or immunofluorescent (IIF) staining using specific antibodies. These advanced tests are available in only a few specialized laboratories, including the CDC.
Treatment for PAM requires immediate and aggressive therapy with a combination of antimicrobial medications. The current recommended regimen often includes:
- Amphotericin B (intravenous): An antifungal medication considered the cornerstone of therapy.
- Miltefosine (oral): A newer drug that has shown promise and is effective against free-living amoebae in lab settings.
- Fluconazole: An antifungal that can provide additional benefit and penetrates the central nervous system well.
- Azithromycin: An antibiotic.
- Rifampin: An antibiotic.
In addition to drug therapy, aggressive supportive care is vital, including measures to manage brain swelling, such as therapeutic hypothermia (cooling the body below normal temperature).
Despite these treatments, the prognosis for PAM is extremely poor. The fatality rate is shockingly high, exceeding 97% to 98.5%. Only a handful of individuals worldwide have ever been reported to survive PAM. Early diagnosis and immediate, aggressive treatment are critical for any chance of survival.
The Rarity: Putting the Risk in Perspective
While the thought of a "brain-eating amoeba" is terrifying, it's essential to understand just how rare these infections are. Naegleria fowleri is commonly found in warm freshwater environments, yet human infections remain incredibly uncommon.
Globally, only 381 cases were reported between 1937 and 2018. In the United States, between 1962 and 2024, there were only 167 reported cases, with fewer than 10 occurring annually. To put this into perspective, you are far more likely to die from drowning than from a Naegleria fowleri infection.
Most cases in the U.S. occur in southern states during the summer months (July, August, and September) when water temperatures are highest. Young boys appear to be disproportionately affected, possibly due to engaging in more vigorous water activities that allow water to enter the nose, or playing in sediment where the amoeba may reside. Recent years have also seen cases reported in more northern states, a trend that may be linked to rising water temperatures due to climate change, creating more favorable environments for the amoeba.
Prevention is Key: Staying Safe
Given the rarity and severity of PAM, prevention is the most effective strategy. The good news is that preventing infection is straightforward if you take sensible precautions:
- Avoid certain water activities: Limit or avoid swimming, diving, or vigorous water sports in warm freshwater lakes, rivers, and hot springs, especially during periods of high water temperatures and low water levels.
- Protect your nose: When in warm freshwater, hold your nose shut, use nose clips, or keep your head above water to prevent water from going up your nasal passages. Avoid disturbing the sediment at the bottom of shallow, warm freshwater bodies, as Naegleria fowleri is more likely to be found there.
- Use safe water for nasal rinsing: If you use a neti pot or other nasal irrigation device, always use distilled, sterile, or previously boiled and cooled water. Never use untreated tap water. Boil tap water for at least one minute and let it cool before use.
- Maintain swimming pools and spas: Ensure swimming pools and spas are properly cleaned, adequately chlorinated, and well-maintained to kill the amoeba.
- Flush stagnant hoses: Before allowing children to play with hoses or sprinklers, flush out any stagnant water, especially if it has been sitting in the sun, as this water can reach temperatures suitable for the amoeba.
- Seek medical attention promptly: If you or a loved one experience sudden onset of fever, severe headache, vomiting, or a stiff neck after being in warm freshwater or using untreated water for nasal rinsing, seek emergency medical care immediately. Early diagnosis and treatment, though rare, are critical for any chance of survival.
Conclusion
The "brain-eating amoeba," Naegleria fowleri, is a stark reminder of the hidden dangers that can exist in our natural environment. While the risk of infection is exceedingly low, the consequences of Primary Amoebic Meningoencephalitis (PAM) are devastating. By understanding where this microscopic menace lives and how infections occur, we can take simple yet effective measures to protect ourselves and our loved ones. Remember, awareness and caution, not panic, are your best defenses against this rare but deadly threat. Enjoy warm weather and water activities responsibly, and prioritize safe water practices for nasal hygiene.